Medical software design has grown up, moved out, and left the clinic behind. With the application of new technology, innovative software products are shifting our healthcare experience from the traditional episodic doctor-in-clinic context to one where healthcare is an omnipresent part of our everyday lives.
Our healthcare interactions now include a breadth of new experiences like smartphone apps, connected devices, retail interactions, home health delivery kits, and telehealth video conferencing. Patients have come to expect that healthcare will meet them in their homes and on their phones.
As patient touchpoints and care expectations evolve, the medical device industry will need innovative ways to consistently deliver value. One helpful starting point: look at industry trends to understand how other leaders are addressing the needs of patients and providers.
Here, let’s look at three trends—everyday software integration, task automation, and personalized care—that are shaping software design for medical devices.
Trend #1: Weaving medical software solutions into everyday life
Now more than ever, software design for medical devices must focus on the patient experience in the context of everyday life. A recent innovation in diabetes management is a great example of how the software operating medical products should be designed to fit seamlessly into patients’ daily routines.
Historically, the care protocol for a Type I or Type II insulin-dependent diabetic was intense. It required frequent manual blood glucose monitoring, food and exercise tracking, and self-injections of insulin.
The daily task list for a patient was time consuming and disruptive. A person with Type I diabetes, for example, may have needed to self-inject insulin three to four times a day. They may have also needed to do finger-prick blood tests to measure blood glucose levels before each meal and before bed.
Thanks to technology, diabetes management has come a long way. But with so many moving parts, the daily mental load of diabetes management can still be draining. Regular injections and blood glucose monitoring can create feelings of embarrassment and shame, especially in public. Those feelings contribute to a mental health crisis among people with diabetes: compared with non-diabetic individuals, they’re two to three times more likely to have depression.
Despite these challenges, it’s important to understand the consequences of mismanagement: strokes, heart attacks, and kidney failure, all of which can be fatal. To avoid these complications, diabetes patients need digital health solutions that make it easier to manage their condition.
The good news: over the last few years, several medical device companies have developed innovative products that streamline the diabetes management experience and deliver better outcomes. A few highlights:
Sensyne: In 2020, Sensyne released a digital health app that enables providers to view patients’ self-reported blood glucose levels in real time. Providers can then suggest insulin dose modifications via push notification.
Tandem: Tandem’s connected diabetes management system combines an insulin pump, mobile app, and web app to enable insulin administration from a patient’s phone or laptop. The app also provides patients with dashboards to view trends over time.
Glooko: Glooko’s digital health app syncs a variety of data (fitness, nutrition, insulin, continuous glucose monitor, etc.) from popular apps like Apple Health and Fitbit to give patients a more holistic view of their diabetes management.
The throughline with each of these products: they take a user-centric approach to product development. Each product took into account existing patient pain points, like embarrassing shots in public or needle fatigue. What’s more, each product accounts for the provider’s experience as well—there’s a clear emphasis on easy-access, integrated patient data that can inform care recommendations.
With a user-focused design methodology, the medical device industry can streamline workflow and functionality for patients and clinicians. The time and mental energy a patient diverts to data entry can be more potent when it is conserved to focus only on behavior change.
Trend #2: Automating tasks to save time and boost patient adherence
Automation does the work that needs to be done without being asked. There are familiar examples of automation like digital alerts, reminders, and notifications that all work behind the scenes to make life easier. But there are also newer automations like medical supply re-ordering, real-time prescription adjustments, or appointment scheduling that execute more complex tasks without human initiation.
Given the current state of the healthcare industry, automation may be more important than ever. There’s a widespread staffing shortage, in part due to a simmering burnout crisis. Earlier this year, the US Department of Healthcare and Human Services urged industry leaders to automate more administrative processes as part of a national initiative to slash burnout by 75 percent by 2025.
For the medical device industry, it’s clear that now is the time to deliver automation-focused digital health solutions. Automated tasks can save providers time on administrative tasks, easing their day-to-day burden and giving them more time to engage with patients.
Of course, automation doesn’t just benefit providers. For patients, automated appointment scheduling or treatment reminders can promote adherence to their treatment plan. Adherence is a critical indicator in influencing and predicting success of a care protocol and improving patient health outcomes.
Before starting product development and design, it’s important not to rely on assumptions about what patients and providers want automated. Instead, conduct user interviews that paint a nuanced picture of their needs. As you spend time with users, you’ll have a better understanding of which tasks are most draining, time consuming, or easily forgettable.
When we’ve asked patients why they skip important parts of their care plan, they often give reasons like “I forgot,” “I didn’t realize,” or “It just isn’t part of my regular routine.” These answers signal a need for automated solutions like step-by-step care reminders or prescription refill notifications. Any time a task can be defined in terms of a checklist or parameters (e.g., “take these three medications every morning and evening”), there is an opportunity for software to automate its facilitation, which improves both usability and outcome metrics.
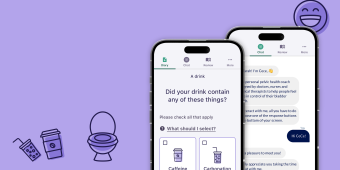
In our own product development, we designed a chatbot for digital therapeutics firm Renalis to automate engagement with patients with overactive bladder (OAB). The patients were part of a study that required keeping a bladder diary over an eight-week period.
Ordinarily, providers might call or email patients to boost adherence. With our chatbot, CeCe, we wanted to encourage self-driven adherence by automating in-app communications and streamlining the diary entry process.
In our user interviews, we learned that OAB is an emotionally fraught condition for many patients. Without a friendly app experience, engagement would suffer.
From that information, we knew we needed to design an automated chat experience that didn’t feel blunt or robotic. We designed the chatbot to be gentle and conversational, with a mixture of text, emojis, and inviting color palettes to ease the user into the experience. Then, we checked in with users at every stage of the design process to make sure their needs were being met. As a result, we delivered an inclusive, user-first automated tool that boosted patients’ adherence.
Trend #3: Personalizing the patient experience to improve healthcare outcomes
A stumbling point for automation is often that a one-size-fits-all approach ignores the highly personal nature of each patient’s journey. As a result, the patient experience suffers. Software-driven personalization can pick up the slack by applying data about a specific individual to make a custom recommendation.
For many providers, clinical decision support (CDS) software can help personalize the patient experience at the point of care. CDS tech works by analyzing EHRs and other inputs to enhance automated tasks and customize treatment plans. For example, a CDS tool can compare patient symptoms to historical data to make more accurate diagnoses. Another tool might use fitness tracker activity to automate patient communication via a MyChart integration.
CDS-powered personalization holds massive potential for the medical device industry. It’s behind bleeding-edge advancements in the precision medicine IoT.
Tempus, for instance, uses genetic data and artificial intelligence to help oncologists create the care protocol that will be most effective for a specific patient. Its digital hub allows providers to view each patient’s genomic profile within the context of their care history. The software also integrates with oncology databases to enable more powerful treatment recommendations. And in 2021, Tempus announced an “Alexa-like device for doctors” that provides insights in real time.
Personalization tools like these are at the forefront of the medical device industry—and the patient impact is real. A personalized care experience can help patients feel seen and understood as individuals as they navigate their care.
For a weight loss surgery patient, for example, a provider might develop a tech-enhanced recovery plan that includes local resource suggestions, meal plans responsive to dietary restrictions, age-appropriate rehab exercises, and a wearable fitness tracker to count steps. This plan isn’t one-size-fits-all. The patient can trust that their provider is delivering high-value care that’s specific to their needs.
Just like a tailored outfit, patients routinely reach for a personalized solution because it wears well. Once worn, a solution’s influence on goals like behavior change can be slipped into the jacket pocket.
Another benefit to personalization: it can directly impact healthcare outcomes. As an example, let’s return to the surgery patient scenario. Their fitness tracker can relay step count data to their provider via MyChart. If the provider notices a downward trend in daily steps, they can use a CDS tool to automatically send a recovery plan reminder and ask about any exercise barriers.
With more personalized data, the provider has both a leading indicator of potential problems and the opportunity to address those problems before they cause damage. That intervention helps improve adherence, which will lead to better health outcomes.
Personalization can empower patients to take control of their own healthcare. But to create lasting behavioral change, it’s important to design with patient education in mind. And that educational component must lead with empathy.
We’ve seen the impact of personalized, empathy-first education in our own product development. In the previous section, we mentioned how we designed CeCe to automate engagement with OAB patients. That included two key functions: educating patients about their condition and providing them with exercises to practice.
Crucially, patients needed to receive this information in a way that helped them feel personally cared for. That’s because OAB can be a highly stigmatized condition, and patients often carry a lot of shame about their symptoms. After talking to users about their experiences with their condition, we chose to implement friendly, inclusive, and jargon-free language throughout the app. The result: an empathetic educational experience that was tailor-made for people with OAB.
A promising future for medical software design
As digital health solutions continue to evolve, these trends will remain in focus as ways to support behavior change and drive health outcomes. Innovation, however, does not stop here.
As solutions evolve and artificial intelligence continues to make gains, we will see new and more creative features within these themes that integrate, automate, and personalize in ways we cannot even imagine today.
No matter what tech is trending, we’re serious about grounding our product design in a human-centered approach. It’s core to our design thinking methodology, and it’s key to maximizing value for our client partners and users.
Want to learn more about how we’re designing digital health solutions? Let’s have a conversation—we’d love to hear from you.