Remote patient monitoring (RPM) has enormous potential to improve health outcomes. By tracking physiological indicators on an ongoing basis, RPM solutions make it possible for clinicians to get a longitudinal view of their patients’ wellbeing, which significantly increases their ability to recommend therapeutics and treatment plans to improve health.
That vision can only be realized, though, when patients regularly engage with RPM solutions, meaning that they use them as directed so the solutions can gather enough data to accurately represent a patient’s condition.
A key challenge for those developing RPM solutions, then, is finding ways to inspire patient adherence. To do that, innovators must start with empathy. Here’s what that looks like in product innovation for the RPM space.
Listen to what users don’t say
Listening to users is both a tenet of product innovation generally and a key part of applying product innovation to the digital health space. Just as important, though, is listening to what users don’t say.
For example, when we were talking to patients during user research for our work with Renalis to develop an RPM solution for people with overactive bladder (OAB), we were struck by the way they characterized their experience of the condition.
A typical response went something like this: “Oh, it’s not really that big a deal for me.” And then they’d go on to describe many ways in which OAB affected their daily life and forced them to change their behavior.
That was a big ah-ha moment for us. It highlighted the extent to which embarrassment and shame about symptoms affect a person’s willingness to acknowledge them, to the extent that people whose daily lives were greatly impacted by OAB had convinced themselves that it “wasn’t that bad.”
The implications of having a stigmatized condition (or one with stigmatized symptoms) are huge. If users were reluctant to say something to us, when we’d called specifically to talk about their condition, how likely were they to mention their experience to their doctor, in a situation where they’d have to bring it up proactively?
One of the first things we have to recognize in developing RPM solutions is that even acknowledging having certain conditions requires a big effort for some patients. The solutions we build to help monitor these conditions have to do everything they can to validate the patient’s decision to take action.
Acknowledge the role of emotions in adherence
Researchers recognize that patient beliefs and attitudes affect their adherence to treatment protocol. But many typical treatment plans don’t actually take beliefs and attitudes into account in any meaningful way.
In many healthcare settings, it’s common for a clinician to view diagnoses and treatments in purely physiological terms, without recognizing the emotional component of adhering to a treatment plan.
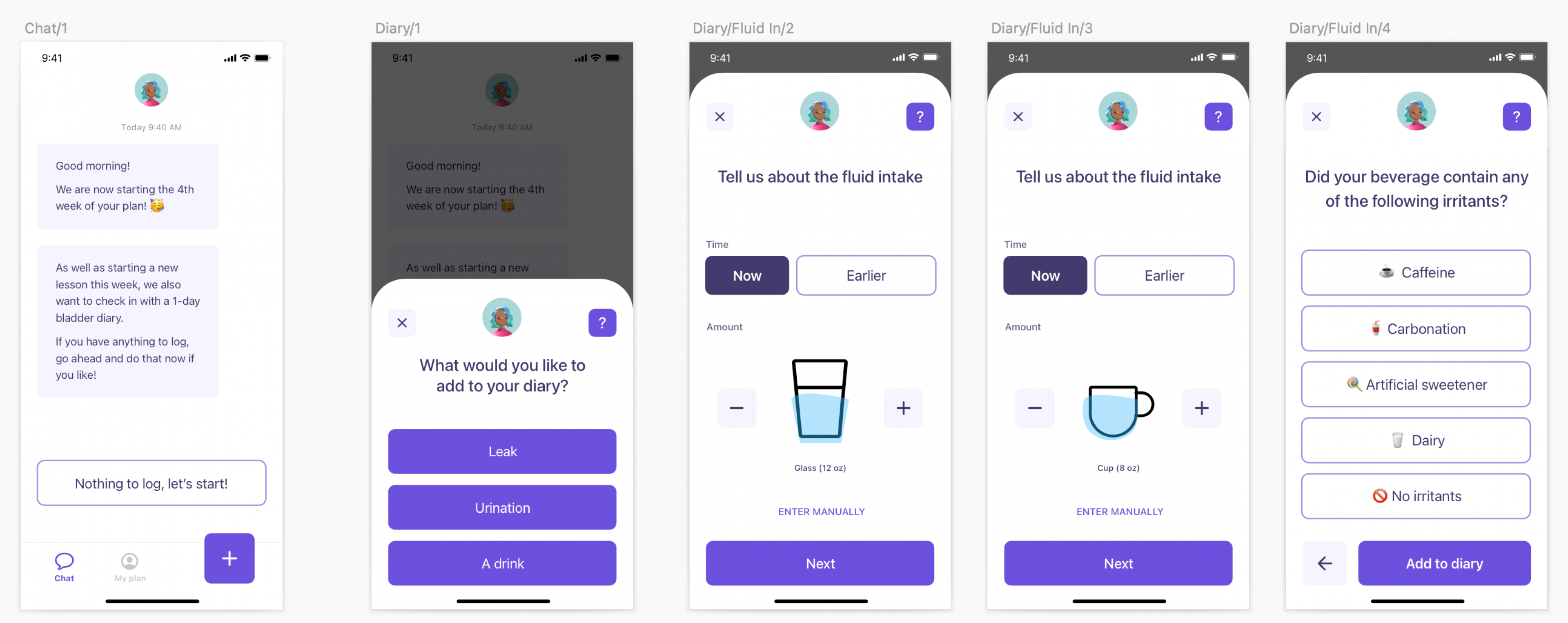
For OAB, common treatment protocols include…
- Keeping a bladder diary.
- Doing pelvic health exercises.
- Engaging in some kind of behavioral therapy.
If a patient doesn’t adhere to that treatment plan, it raises a red flag for clinicians to understand the reasons why. This is really important, as it opens the window for innovative approaches beyond what Western medicine typically calls for.
Given what we discovered about the embarrassment many patients felt about their OAB symptoms and knowing how that negative emotion could affect their adherence to a treatment plan, we determined that the RPM solution we developed for Renalis had to find ways to help minimize users’ embarrassment.
Why? Because when patients feel good about engaging with their bladder diary, they’re more likely to do it. And that means more data, which means a more accurate picture of their health, which means better treatment from their clinician.
It’s hard to overstate how important this concept is when applying product innovation to RPM solutions. Think, for example, of all the health conditions affected by diet and activity levels, and how much emotional baggage people often have around those two things. The good news is that RPM solutions are uniquely positioned to help address those complex feelings to drive better outcomes.
Acknowledge (and leverage) the power of stories
I can tell you all day that one in three people in the United States has a pelvic health disorder. But what happens when I mention that my neighbor didn’t go to her favorite vacation spot for 15 years because her OAB made her worry that she wouldn’t be able to handle the four-hour drive? Suddenly, when we communicate via story, the impacts of OAB are personal. We see how they impact someone’s life.
This isn’t a fluke of my neighbor or of OAB. Research about the power of stories shows that they are an essential part of our humanity. One thing they’re particularly good at is eliciting empathy (we can’t help but picture ourselves similarly unable to visit our favorite place, and that affects us).
In the RPM solution we built for Renalis, we realized we needed to help patients develop empathy for themselves and their symptoms and broaden awareness about the power of empathy among clinicians. We leveraged stories to help achieve that.
For example, when a patient adds information about a bladder leak to the app, we offer contextual feedback. Sometimes we use statistics (70 percent of people have a leak after an experience like that) and sometimes we use stories.
We also thought about the larger story that the app helped users tell themselves about their condition. Besides making it easy and even pleasant to use, we wanted everything about the app to work toward destigmatizing OAB and its symptoms. To achieve that, we…
- Used matter-of-fact language instead of medical jargon.
- Used clean lines and lively icons to create a friendly look and feel.
- Combined icons with text to enhance clarity.
- Used gender-inclusive language.
The overall story of the app is that OAB is a normal part of everyday life. When users internalize that message, they’re much more likely to feel good about using the app to track their symptoms and therefore provide the data their clinicians need to assess their progress and recommend next steps. And it all starts with empathy.
RPM solutions should treat people, not conditions
There are countless health conditions today that we understand well enough to know the what of treatment. RPM solutions have the potential to expand our knowledge even further.
But we often fall short on the how, and particularly on how to motivate people to adhere to treatment plans we know can work.
Empathy can close the gap. When we accept that people’s emotional realities affect daily behavior and design health solutions that work with those realities, we’re able to create solutions that treat the entire person and lead to better health outcomes.
If you’d like to hear more about how empathy can lead you to better outcomes, let’s get in touch.