Remote therapeutic monitoring (RTM) and remote patient monitoring (RPM) services are poised to transform the field of digital health in the coming years, thanks to new CPT codes that let clinicians get reimbursed for prescribing these solutions, among other market forces.
The power of these monitoring solutions lies in their ability to both motivate patients to adhere to treatment protocol and track that adherence to generate a rich source of valuable health data—two features that, together, create a closed feedback loop.
As we’ve mentioned elsewhere, the data that RTM and RPM services generate will have a transformative impact on the healthcare industry, allowing clinicians to track the success rate of various treatment plans for people with a number of physiological characteristics. Ultimately, clinicians will be able to prescribe treatments with much greater confidence in their likely outcomes.
In this piece, I’ll dive into why that’s true, examining key lessons from our past work developing remote patient monitoring solutions and the advantages of those solutions that work uncovered. But first, let’s look a bit closer at what remote patient monitoring is, plus some real-world examples that illustrate its impact.
Background: What is remote patient monitoring?
Remote patient monitoring services combine wearables and digital applications to collect physiologic health data and power data-driven insights. They’re often used to monitor patients with chronic conditions like hypertension or COPD. When used alongside other telehealth solutions (e.g., virtual care appointments), RPM can provide patients with a more accessible alternative to in-person visits, particularly for people with complex care needs and those in rural areas.
While many RPM solutions have been on the market for years, the COVID-19 pandemic drastically accelerated adoption timelines. By the end of the first pandemic wave, over 40 percent of patients had delayed or avoided their care—especially if they had a chronic condition. But without consistent medical attention, these patients risked worsening their condition and suffering serious complications.
To help patients remotely manage their care, many providers turned to RPM services. The long-term projection? By 2025, over 70 million patients in the US will likely use RPM tools as part of their care plans.
What are some commonly used RPM tools? One example is a connected glucometer, a type of wearable that tracks blood glucose levels for patients with diabetes. It transmits that data to a shared digital platform, where patients and providers can view blood glucose levels over time.
Instead of relying on self-reported data—which might vary based on the patient’s recording consistency—providers can access real-time, auto-transmitted data that can inform their care recommendations. If a patient’s blood glucose has spiked, providers can send a push notification to suggest a modified insulin dose.
When patients use RPM solutions, there’s a clear impact on health outcomes. For instance, the University of Pittsburgh Medical Center integrated RPM tech into care plans for patients with congestive heart failure. Over a year and a half, providers found that…
Over 90 percent of patients adhered to their care plan.
Over 90 percent were highly satisfied with their patient experience.
Hospital readmissions dropped by 76 percent.
At TXI, we’ve designed RPM software with a focus on boosting outcomes for the patients our partners serve. In the next few sections, I’ll highlight four lessons from this work.
Lesson 1: Remote patient monitoring services must work for patients AND clinicians
Anyone looking to develop an RTM or RPM solution that enjoys high adoption has to cater to two key stakeholders:
The end-user or patient: You have to demonstrate to this group that the solution is helping them so that they use it.
The clinician or prescribing member: You have to convince this group that yours is the correct solution to use in a competitive space.
The key to convincing both parties is to create patient engagement feedback loops that inspire adherence.
Let’s look at an example.
Medical device developer Theragen asked us to design an RPM solution that would pair with ActiStim-S, a noninvasive therapeutic that delivers electrical signals to help stimulate bone growth after vertebrae fusion surgery. Our goal was to help improve adherence to a treatment plan that can often be exhausting.
For the best outcomes, patients need to continuously wear the ActiStim-S device for between six and nine months. To keep adherence from tanking, we needed a solution that accounted for patients’ unique needs—and gave providers the right patient data.
In talking to clinicians and patients, we learned two critical pieces of information:
First, that movement is key to recovery from surgery.
Second, when patients are in post-op pain, they’re more likely to be still.
Finally, we discovered that patients have a very short-term memory for pain, meaning it’s hard for them to assess their current pain relative to their past pain.
That’s a big problem for a population that only interacts with their surgeons at multi-week intervals after surgery. Without any way to daily track non-physiologic data such as pain levels, it’s almost impossible for the clinician to measure the success of the surgery during the recovery phase and therefore to know what patient care steps to recommend to advance their recovery.
Remote patient monitoring solutions have a significant advantage in scenarios like this because they enable data tracking over time.
The solution we developed for Theragen (an app to accompany the therapeutic device) taps into this advantage in three key ways:
It prompts users to keep a pain diary. This lets them see how their symptoms improve over time, which helps motivate them to stick with the treatment.
It tracks step-counting data from the pedometer Theragen built into its device. This lets patients observe how their movement correlates with pain.
It makes data shareable with clinicians. Today, patients’ pain diaries, step counts, and device usage are downloadable via PDF for clinicians, who can use this information to track a patient’s progress in recovery and guide their next-step recommendations. In the future, we’re considering a patient portal or EMR (electronic medical record) integration that would give clinicians a real-time view of patient data.
This leads directly into the second big lesson.
Lesson 2: Data is an essential ingredient to success
There are a few ways to look at the success of an RTM solution like what we built for Theragen:
Success for the individual patient: is the solution helping them stick with their recovery protocol and leading to better health outcomes?
Success for the solution itself: does it improve adherence in a way that’s demonstrable to clinicians and repeatable for other patients?
Population-level success: can we demonstrate to enough people that the solution improves outcomes for a given group so that it becomes widely adopted, thus improving outcomes for nearly everyone in that population health group (and often lowering healthcare costs)?
All three of these require data. To be successful, RTM solutions must make it easy to gather data on an ongoing basis.
More than that, though, RTM solutions should make data visible and understandable to both physicians and patients. It’s one thing for a surgeon to tell you to be sure to move around as much as possible; it’s quite another to see that the days with the highest step counts consistently have the lowest pain ratings.
That can lead to the kind of ah-ha moment that makes the difference between a patient adhering to surgery recovery protocol and not.
In our work with Theragen, we found that the RTM component of its product offers a considerable advantage over similar products in that it is easier to use, inspires movement by tracking steps, and leads to better adherence.
Data visibility isn’t the only thing that inspires adherence, though.
Lesson 3: Emotions affect adherence
One of the most fascinating and important takeaways from our user research is that the way people feel about their condition affects the likelihood of adhering to a treatment plan.
This is especially true for conditions that have social stigma, like overactive bladder (OAB). People with OAB often feel so embarrassed about their symptoms that they never bring them up, even with their doctor.
As you can imagine, that makes OAB really hard to treat.
Because even if a person does talk to their doctor and gets a treatment plan (keep a diary, take medicine, do physical therapy), their adherence has a huge psychological component.
A remote patient monitoring program has the potential to address that psychological component to maximize adherence and improve outcomes. To illustrate, here’s an example from our work.
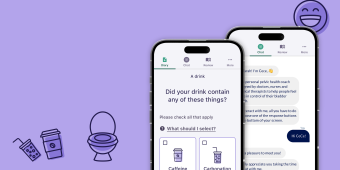
Digital therapeutics firm Renalis asked us to develop an app that delivers behavioral therapy to treat OAB. Their goal was to use this app as part of a proof of concept study for FDA review. We focused on finding ways to reward patients for engaging with the app and on removing the stigma around the condition.
One use case: When a user reports a leak, the app might offer statistics to show how common such leaks are or share other users’ stories or messaging opportunities to communicate that the user is not alone.
This is a huge advantage of remote patient monitoring solutions. Because patients access them from devices they carry in their pockets or purses, the experience of using them is incredibly intimate. And just as we get small hits of dopamine from seeing someone like our posts on social media, RTM solutions can deliver positive feelings by rewarding users for inputting data and reinforcing that their symptoms are normal and that they’re making progress.
This capability is especially important when patients have limited access to healthcare providers.
Lesson 4: Many patients don’t have access to specialists
A recent McKinsey report projected that remote patient monitoring services could save anywhere from $1.5 to $3 trillion in global healthcare costs by 2030.
That’s a staggering number, but it starts to come into focus when you consider that most people with OAB, for example, don’t live within four hours of a specialist who can diagnose and treat the condition. Others may be closer but physically unable to visit. And others still may be able to visit a doctor for an assessment but not have access to care again until they’ve reached the point of needing surgery.
For anyone with limited access to treatment, symptoms often continue to get worse and worse, affecting their lives in bigger and bigger ways. If and when they are able to get treatment, they typically require more expensive, more invasive procedures (like surgery) than they would have if they’d had access to their care team sooner.
Remote patient monitoring services help solve this. They can be downloaded as part of their care plan by anyone with a smart device and an internet connection. And they don’t just deliver care every few weeks or months, as a specialist would. They can provide prompts, reminders, and reinforcements that improve patient adherence to treatment protocol on an ongoing basis, which can keep patients out of doctor’s offices, and even out of operating rooms.
A major opportunity to improve patient outcomes
Digital health is at an inflection point.
With widespread mobile device ownership and internet access, plus CMS support for remote patient monitoring and remote therapeutic device reimbursement, the potential to transform people’s lives and our healthcare system is tremendous.
When healthcare and digital health companies build solutions that are easy and enjoyable for patients to use, that capture data on an ongoing basis, and that make those metrics accessible to physicians as part of the healthcare delivery process, they’re helping to realize that potential.
If you have a vision for improving health outcomes, we’d love to help you make it a reality. Get in touch, and we can help you figure out where to start.