According to the American Medical Association’s Return on Health Report, digital health companies have received over $100 billion in venture funding since 2010. And while the majority of this investment was made in response to the COVID-19 pandemic, the long term benefits are unsurprisingly proving evergreen.
At the same time, there are a number of roadblocks that keep digital health tools from being integrated into the technologies providers rely on to support efficient patient care plans.
From EHRs (electronic health records) and patient portals to remote therapeutic devices and chatbot automation, such concerns in large part focus on data privacy and security. But a lack of standardization across healthcare organizations and networks also has an impact. As do human factors, like peoples’ comfort-levels using new therapeutic tools.
While there’s no silver bullet for solving inefficiencies in healthcare, proactive engagement is a good start. Luckily, the digital products that help provide positive patient experiences can also help patients and their providers remain collaboratively engaged in the complex process of navigating comprehensive care.
In this piece, I’ll look at how collaborating through digital health technologies can help providers usher patient engagement into a healthier future.
Digital health tools efficiently power positive patient experiences
From remote monitoring devices (RMDs) to electronic health records (EHRs), digital health engagement encompasses a wide range of therapies and apps aimed at improving the patient experience. And the goal, of course, is for improved patient engagements to deliver improved health outcomes.
The transition from paper documentation to widespread use of EHRs, for example, shows how quickly emerging digital health technologies can influence and support the delivery of efficient, effective patient care.
But digital health technologies also offer benefits for the providers delivering that care.
It doesn’t take much effort, after all, to recognize how much easier it is for physicians to review location-neutral, digital health records rather than requesting copies of paper charts from individual providers.
But provider engagement isn’t the only benefit. Digital solutions also make it easier for patients to actively participate in their care. Combined with the increasing prevalence of online patient portals, EHRs make it easy for patients and practitioners to work together through …
Telehealth: The use of digital technologies, such as video conferencing and secure messaging, increasingly offers location-neutral access to personalized healthcare.
Remote therapeutic monitoring: The use of wearable devices and sensors to track patient health data, can support the development of individualized protocols (patient-specific insulin therapy, for example).
Digital health apps: Mobile apps that help patients manage their health, such as tracking medication schedules, monitoring symptoms, and contacting their healthcare providers. Such information offers patients windows into understanding their care, and even incentivizes sustained engagement.
But realizing the benefits of digital health technology isn’t without its challenges. Next, let’s take a deeper look into digital tools like telehealth platforms.
Direct communication channels facilitate more engaged care
Medicine is a two-way street. The long and short of it is, for healthcare to work efficiently, patients need to learn from their providers, and providers need to understand their patients. To put it another way: effective care is engaged care. To expand on this idea, let’s examine the recent popularity of telehealth services.
Though the roots of telemedicine reach back to the mid-20th Century, it’s no secret that the COVID-19 pandemic dramatically increased the need for remote healthcare.
Some providers, however, were at first slow to adopt telemedicine in their practices. But no matter the reason for their initial resistance, inspiring providers to offer remote care to patients became paramount during the pandemic. Doing so not only made it easier for patients to receive care. It lowered the number of patients visiting clinics in person.
In the most dire months of the pandemic, telehealth helped patients remain engaged with care teams they wouldn’t otherwise have been able to see. And by attending appointments remotely, telehealth patients also increased the chances the patients in need of critical in-person treatment could get the care they required.
Today, the benefits of telehealth continue to pay dividends for providers and patients alike. Patients feel more connected to their providers, who are in turn more readily able to answer simple questions, like whether statins interact with Paxlovid, via patient portals.
Data puts patient care journeys into context
We’ve written before about the importance of viewing digital health data not as a result, but as a feature. And that holds just as true for prescribed therapies, like Theragen’s ActaStim-S, as it does for more broadly available consumer tech.
Today, digital technologies like accelerometers are ubiquitous features of personal devices like cell phones and smartwatches. As a result, anyone with a smart device has the option of tracking how many steps they’ve taken in a day, then viewing charts of that data over time. It’s now common to use this feature to track health and set personal fitness goals.
But taken at face value, the fact that someone is logging 10,000 steps per day isn’t particularly helpful. Combine the data reflecting those 10,000 steps with data about that person’s resting heart rate and its change over time, however, and the result could have outsized impact.
The key: this data needs to be…
Clean. Recognizing how to identify the signal from the noise is central to delivering effective care.
Communicated. If data suggesting someone has an increased risk of heart attack isn’t communicated back to a provider, it doesn’t do any good.
Contextualized. Patients may be unaware of risks because they don’t understand what their data is able to tell them about their overall health.
The upshot? With the right approach, data can help incentivize patients to take an active role in their care. And it can empower care teams with the information necessary to understand a patient’s unique circumstances and develop the most appropriate path forward.
New technologies increase the impact of engagement
Advancements in artificial intelligence (AI), like ChatGPT and Elicit’s AI research assistant, promise to significantly increase the possibilities for how providers achieve clinical outcomes and patients proactively engage with and understand their own care.
Consider, for example, how conversational AI could help a provider more quickly navigate critical caregiving reference points like PubMed. Rather than manually searching through a database during an in-clinic appointment, a provider could…
Query the conversational agent about various diagnostic determinants, such as age, medication history, and family health history.
Refer to AI analysis of these cross-referenced determinants to quickly recognize patterns and the corresponding possible diagnoses.
Again, context is key. With this information readily available, providers can then combine it with their contextual understanding of the patient, such as whether they’re in obvious distress or seem to be experiencing a health issue they aren’t reporting. Then, with the whole picture in mind, they can develop the care plan most appropriate at that time.
Next, let’s review a case study detailing how patients can use digital health apps to strengthen the benefits of the treatments their physicians prescribe.
The benefits of successfully engaging with digital health technologies
Though the capacities of ChatGPT and its emerging competitors are captivating, the fact is, like telehealth, conversational AI isn’t a brand new technology. In fact, the benefits of conversational agents (often referred to as chatbots) have for several years been a mainstay in customer service.
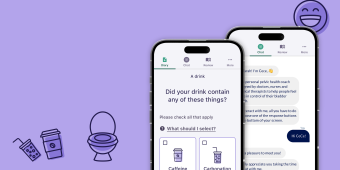
But chatbots have been used to previous success in healthcare, too. And TXI’s work with Renalis Health, for example, shows how building additional functionality into digital health apps like chatbots can drive the heightened engagement that improves patient experiences.
Renalis Health’s chatbot, CeCe Lite, provides people with insight into five days of their personal experiences, helping to educate them about their health. But Renalis Health found it difficult to drive engagement for patients experiencing health issues, like overactive bladder (OAB).
The reason was clear. While OAB may not cause physical pain, it often causes significant psychological and emotional stress. As a result, many pelvic health patients don’t engage with treatments (digital health apps or otherwise) that could relieve their symptoms.
To address this, TXI developed a method for patients to contextualize their experiences. Knowing that their symptoms aren’t uncommon helps relieve the shame associated with seeking care. One-third of patients, for example, experience incontinence after giving birth.
Simply put: pelvic health patients are alone in their experiences. And likewise, few are alone in experiencing shame around the process of their care. But TXI knew that if we could help educate patients about their experiences in the context of others who share their condition, they’d likely become more engaged with the treatments that could provide relief.
So we started by presenting patients with their own data, giving them a window into their progress over time. And by aggregating anonymized datasets to display the cause and effect information about incontinence, we began building the types of features patients could engage with in order to ease their minds.
Collaboration is the key to innovative healthcare
The clinical opportunities that digital health technologies and workflows offer may not be new. But they’re increasingly relied on to deliver care. And as they continue to develop, innovative care teams and their patients are sure to realize further benefits of engaging with digital health apps.
That’s no surprise. Patients and providers alike want treatments that improve well being and help make care journeys as painless as possible. But innovation is about balance. And that means valuing the needs of stakeholders across healthcare equally.
When patients and providers are instead equally engaged in the care journey, they’re more likely to arrive at workable solutions that improve overall health. For their part, this works best when patients are empowered to avoid assuming they are alone in their pain. Likewise, providers can best serve patients by dispensing with a one-size-fits-all approach to care.
Interested in collaborating with TXI to work toward a healthier future? Get in touch.